06 Mar Stress and Seizures in Adults: Is There a Connection?
Does Stress Cause Seizures in Adults?
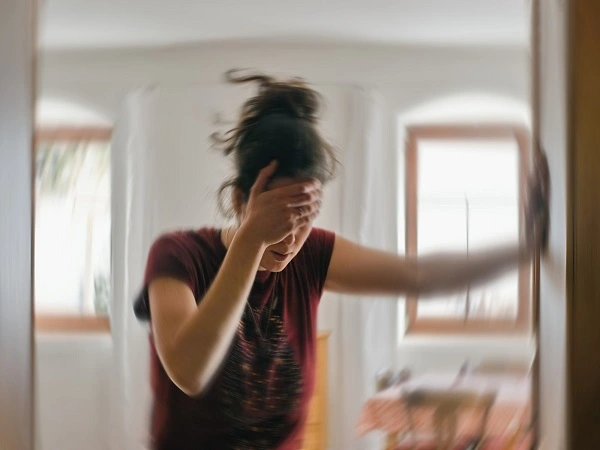
Stress impacts each person differently in our everyday lives. While some individuals may perceive it as a minor inconvenience, it can lead to significant health issues.
Stress isn’t just about feeling a little irritable or uneasy – it can have serious consequences.
Many adults wonder – ‘can stress cause seizures in adults‘.
This curiosity drives us to explore the connection between stress and seizures in adults.
In this blog post, we’ll delve into the scientific understanding of how stress interacts with brain activity, explore the evidence linking stress to seizures in adults, and discuss strategies for managing stress to potentially reduce seizure frequency.
What Are Seizures?
A seizure is a brief impairment in normal brain functioning due to a disarray in electrical activity.
This abnormal activity can cause disturbances in consciousness, motor activity, behavior, and affect.
Seizures can occur in anyone, but they’re most common among patients with nervous system diseases like epilepsy.
Their severity can range from mild episodes that hardly disturb daily life to severe, generalized episodes requiring emergency medical intervention.
Most seizures are caused by something acute and are unlikely to recur. However, recurrent seizures typically lead to a diagnosis of epilepsy.
Symptoms of Seizures:
The symptoms of seizures depend on the affected area of the brain and the overall pattern experienced during the seizure.
Some general characteristics include:
- Extreme Jerking Movements (Convulsions): A sudden influx of muscle contractions occurring randomly along any muscle group.
- Very Short Duration Confusion or Staring Spells: During which the individual may appear unresponsive and unaware of their surroundings.
- Loss of Consciousness or Awareness: After a seizure, there can be significant variations in the severity of weakness or altered mental state, ranging from a split-second “blackout” to an experience of a few minutes during which the individual is conscious but altered.
- Unusual Sensations: Strange sensory experiences accompanying seizures can include tingling sensations, flashing lights, and inexplicable feelings of déjà vu.
- Rapid Mood Swings: Outbursts of crying or laughing, as well as sudden irritability or fear, can be a crucial part of seizures.
Seizures can be of different kinds, and not all include body movements.
Some seizures might show no clear signs except for mild symptoms like brief confusion or the repetition of a simple action.
Types of Seizures
Seizures are classified based on the part of the brain where they originate and the symptoms they cause.
The primary categories are focal (partial) seizures and generalized seizures.
1: Focal (Partial) Seizures
Focal seizures affect a specific region of one hemisphere of the brain and may involve changes in awareness.
They are subdivided into:
a) Focal Aware Seizures (formerly Simple Partial Seizures):
These seizures do not cause loss of consciousness. Common symptoms include unusual sensations, sudden and unintended emotional changes, or muscle jerking.
b) Focal Impaired Awareness Seizures (formerly Complex Partial Seizures):
These seizures typically involve loss of awareness or consciousness. Observers may notice the person performing purposeless actions, such as lip-smacking, hand-rubbing, or walking in circles, without being aware of their behavior.
Focal seizures may spread to both hemispheres of the brain, evolving into focal to bilateral tonic-clonic seizures.
2: Generalized Seizures
Generalized seizures involve both hemispheres of the brain from the onset and typically result in loss of consciousness.
They are subdivided into:
- Tonic-Clonic Seizures (formerly Grand Mal): These seizures have two phases. The tonic phase involves muscle stiffening, often with a cry and a fall, followed by the clonic phase, characterized by rhythmic jerking movements. Loss of consciousness is common, and post-seizure confusion (postictal state) often occurs.
- Absence Seizures: These brief seizures, common in children, cause a temporary lapse in awareness, often appearing as a blank stare or “daydreaming.” Subtle movements like eye blinking or lip-smacking may occur.
- Myoclonic Seizures: These involve sudden, brief muscle jerks or twitches, typically affecting the arms or legs. Consciousness is usually preserved.
- Atonic Seizures (Drop Attacks): These cause a sudden loss of muscle tone, leading to head drops or falls. They are brief but can result in injuries.
Each seizure type has distinct characteristics, making accurate classification essential for diagnosis and treatment.
Causes of Seizures In Adults
There are many reasons that can cause seizures. One seizure might happen for a single reason, but others can be from ongoing health issues that lead to more seizures.
Here are the causes:
1: Epilepsy
Epilepsy is a condition that causes repeated seizures.
These seizures can happen for different reasons, like genes, injuries, infections, or problems in the brain.
The seizures can happen often and vary in how strong they are, making the condition long-lasting.
2: Head Injuries
The more traumatic brain injuries are received from accidents, falling, or sports activities, the greater the risk of seizures.
Disruption of electrical activity may burn healthy brain tissue and predispose the brain to seizures.
Seizures may occur immediately or soon after the injury or develop in years or months called post-traumatic epilepsy.
3: Infection
Bacterial infections, such as meningitis, encephalitides, or brain abscesses, can cause seizures by affecting the brain.
All these are inflammatory conditions that inhibit the normal function of the brain and create abnormal electrical activity in it.
4: Brain Tumors
Abnormal growths present inside the brain may exert pressure on the already existing tissues and distort or even interfere with the electrical signaling.
Among the earliest signs of a brain tumor, seizure activities can be found. Both benign and malignant tumors can cause seizure activities.
5: Stroke
An interruption of blood flow in a part of the brain leads to the death of its cells.
Tissue scars in the brain may cause seizures after stroke, especially to older persons. Seizures can happen upon the stroke or later as well.
6: Deprivation of sleep
Sleep deprivation lowers the threshold of seizure activity making the brain vulnerable to abnormal electrical discharges.
Conditions like insomnia and sleep apnea heighten this susceptibility.
Hence, regular healthy sleeping patterns are crucial to stopping seizure activity.
7: Withdrawal from Drugs and Alcohol
There will be withdrawal seizures if there is sudden disruption from alcohol or drugs (e.g. benzodiazepines or opioids).
Chronic substance use-induced change in brain chemistry leads to the neurological imbalance after suddenly stopping.
One must be medically supervised during detoxification to prevent seizures.
8: Metabolic Imbalances
The abnormal concentration of glucose, sodium, calcium, or magnesium can also affect normal brain functioning.
Decreased blood sugar (hypoglycemia) is one of the most trigger-inducing states for seizures, more so in those suffering from diabetes.
Dehydration and electrolyte balance defects can also add to the tendency to have seizures.
9: High Fever (Febrile Seizures in Adults)
Adults suffering from very serious infections or high fever are also able to have febrile seizures, although they occur more frequently in children.
The episodes are usually short and self-resolving upon the administration of treatment.
10: Genetic Components
People may genetically inherit a particular tendency toward seizures from their family.
Some mutations in genes may lead to dysregulation of inter-cell communication in the brain, thus predisposing them to seizures.
Definition of Stress and Its Physiological Effects
Stress is the body’s natural reaction to any kind of physical, emotional, or psychological challenges and demands.
It activates the fight-or-flight response within the body, a survival reaction that developed to help a person in the presence of a threat.
Excessive or chronic stress produces negative health effects, particularly on the brain.
How Stress Affects the Body?
Long-term stress can interfere with all normal physiological activities and may be considered one of the potential causes of central nervous system disorders, such as epilepsy.
The following are some of the effects of stress on the body:
- Raises levels of cortisol: Stress turns on the HPA axis, which causes the body to release cortisol, the main hormone for stress. Over time, higher cortisol levels can harm memory, emotions, and thinking. It can also change how brain chemicals work, making brain cells more active and possibly leading to more seizures.
- Affects sleep patterns: Another direct consequence of stress is insomnia or disrupted sleep, both of which are proven seizure triggers. Sleep loss diminishes the brain’s ability to modulate its electrical activity, preventing further possible threshold deposition of seizures.
- Triggers inflammation: Chronic stress increases chronic inflammatory states in the brain and nervous system. Inflammatory responses have been linked to some neurological disorders that classify epilepsy, concerning neural connectivity and excitability levels.
- Weakens the immune system: Stress weakens the immune system, making people more prone to infections that might also trigger seizures. Viral diseases such as encephalitis or meningitis may induce seizures in non-immune adults.
In general, these changes indicate how conditions resulting from chronic stress create an environment that makes the brain vulnerable to seizures.
Common Sources of Stress In Adult Life
Stress encompasses many aspects of everyday life.
While everyone has their own sources of stress, most of the following are common stressors among adults and may all contribute to seizure occurrence.
1. Stress from Work
Working under excessive demands or time limits and sustaining conflicts at work make one increasingly prone to stress.
Job insecurity or anxiety over possible redundancies can keep such stress simmering.
Long hours and burnout contribute to physical and emotional exhaustion, thereby lowering the threshold for seizures.
2. Financial Concerns
Managing rising costs, dealing with debts, or going through sudden debt crises can be overwhelming.
Chronic stress may sometimes emanate from uncertainty about future income and political or economic insecurity.
Financial stress generally disrupts sleep, increases anxiety, and contributes to certain health conditions that correlate with increased seizure risk.
3. Family and Relationship Stress
Intimate relationship conflicts, such as marital or familial disputes, create a lot of emotional stress.
Caregiving—for young children, older parents, or anyone sick in the home—can really take a physical and mental toll on individuals.
These situations can also have a huge impact on a person’s emotional life, and such events can therefore lead to severe emotional distress, which can be a trigger for seizures in susceptible individuals.
4. Health Problems
Chronic diseases, such as diabetes, hypertension, or other neurological conditions, are psychosocial stressors.
Various states of diagnosis-related epilepsy may also increase stress levels related to seizure management, medication side effects, or even stigma.
Pain-inducing diseases or disabilities can lead to depression and anxiety, which can modulate seizures.
5. Traumatic Experiences
This refers to histories of trauma due to childhood abuse, traumatic accidents, and exposure to violence.
Higher neuronal hyperactivity is observed in post-traumatic stress disorder (PTSD), whereby the brain is prepared for seizure activity.
Triggers for seizures may include flashbacks, panic attacks, and extreme emotional reactions.
Stress is closely interconnected with neurological health; thus, the management of daily stress can go a long way in reducing seizure risk.
The Relationship Between Stress and Seizures
The relationship between stress and seizures is significant: can extreme stress cause seizures?
Yes, chronic or intense stress can lower the seizure threshold, and many wonder, does stress increase seizures?
It often does, by altering brain activity and sleep patterns.
Ultimately, while not the sole cause, it’s clear that is seizure caused by stress is a valid question, as stress acts as a major trigger in susceptible individuals.
Let’s break it down.
How Stress Affects the Brain?
Does stress cause seizures? YES! Stress can change the brain to make seizures more likely.
This happens especially in people with existing brain problems. Stress makes your body release hormones.
These hormones affect how your brain works. Your stress system can get overactive. This leads to too much of certain stress hormones.
These hormones can upset the brain’s balance. This balance controls nerve signals. An imbalance can cause nerves to misfire. This increases seizure risk.
Stress also changes brain chemicals. It can raise a stimulating chemical called glutamate. It can lower an calming chemical called GABA.
This makes brain cells more easily excited.
It lowers the point at which a seizure can happen. Nerve cells become more sensitive due to stress.
They can fire too easily and too fast. This high activity often causes seizures. This is more common in people with epilepsy.
Types of Stress That May Trigger Seizures
Not all stress is the same, and different things that cause stress can affect a person’s seizures in different ways.
Here are some common things that may trigger seizures:
a) Emotional stress:
Can anxiety give you seizures? YES! Anxiety, excessive worry or depression and emotional distress can result in being pro-seizures.
A lot of people with epilepsy have spoken about the close connection between intense emotional experiences and seizure episodes.
b) Physical Stress:
Less sleep, greater fatigue, sickness, and activities beyond physical limits can very much be harmful to brain functioning.
Fatigue and sickness will lower the seizure threshold of the brain, opening up possibilities of abnormal electrical activity.
c) Environmental stress:
Bright lights – especially flashing lights for individuals with photosensitive epilepsy – and loud sounds may be enough for sensitive individuals to have seizures.
Extreme temperatures, dehydration, and even outside factors contribute to the person’s increased susceptibility for seizures.
Identifying personal triggers would thus be a priority because different stress approaches would affect individuals differently to prevent them from seizure incidents.
The Role of Anxiety and Depression
Individuals having epilepsy or other disorders related to seizure activity are affected by anxiety and depression.
These two aspects of mental health are likely significant in terms of seizure incidence, as they can:
- Bring about more high stress hormones, contributing to increased neuronal excitability.
- Worsen the sleep pattern and, hence, lower the seizure threshold more.
- Contribute to the failure of taking medication, all of which lead to uncontrollable seizure activity.
A healthy emotional state helps with brain health and can prevent seizures.
Seizures Caused By Stress And Anxiety
Stress and anxiety can contribute to seizures in some individuals, particularly those with epilepsy or other seizure disorders.
Understanding the connection between mental health and seizures is essential for effective management.
Recognizing that stress and anxiety can trigger seizures in susceptible individuals allows people to take proactive steps to manage their mental well-being and reduce seizure frequency.
Consulting healthcare professionals, such as top neuropsychiatrist in Patna Bihar, is critical for developing personalized strategies to address stress-related seizures.
Incorporating stress-reduction techniques, such as exercise, mindfulness, meditation, or other relaxation methods, can help lower the likelihood of seizures.
By prioritizing mental health and adopting effective stress management strategies, individuals can minimize the impact of stress and anxiety on their lives and seizure control.
Statistical Data or Studies Supporting The Connection
Can you have a stress related seizure? So far, many studies throughout the years have proven to explore the connection between stress and seizures.
It does not directly cause epilepsy, but it can lower the seizure threshold and trigger seizures in people who are already prone to them or have other health issues.
Principles of Research
A study done in the year 2021, published in Epilepsy & Behavior, discovered a 60% incidence of stress among epilepsy patients as a seizure trigger.
Chronic emotional stress has a significant role in enhancing neuronal excitability and making the brain susceptible to seizures.
Accordingly, the data showed fewer occurrences of seizures for patients who practiced stress management techniques.
Scientific Research on Stress and Seizures
An area of research identifies psychogenic non-epileptic seizures (PNES) as a distinct entity.
These seizures are nearly similar to epilepsy but are triggered by emotional or psychological stress, not by abnormalities in the brain’s electrical activity.
In such cases, a person develops the general manifestations of an epileptic seizure, but their brain does not actually have any electrical disturbance producing it; it is instead caused by intense stress or a past traumatic experience.
PNES patients are more likely to benefit from psychological treatment, for instance, through Cognitive Behavioral Therapy (CBT), rather than with anti-seizure medications.
A Study in the Journal of Clinical Neuroscience
The present experiment has assessed the effect of chronic stress on brain plasticity, finding that a condition induced by hypercortisolemia might affect neuronal connections, leading to increased seizure sensitivity.
These stress hormones appear to decrease seizure susceptibility but are associated with structural and functional alterations in the brain, especially concerning various forms of memory, emotions, and seizure activity.
Therefore, seizure-prone individuals should adopt stress-management strategies to bolster their neurological health.
Such studies support the close interrelationship between stress and seizures, thereby highlighting the need for stress control among persons with stress-induced seizures or epilepsy.
How To Stop Stress Seizures: Coping Mechanisms and Management Strategies
Does stress cause seizures in adults? Stress can greatly enhance seizure activity while adequate coping strategies can lessen seizure aggravation.
Listed below are stress management activities that can serve to decrease the possibility of having a seizure.
Take a look at the steps on how do you stop stress seizures…
1: Stress Reduction Techniques
Mindfulness meditation helps keep your mind in the present. It reduces negative thoughts.
Studies show mindfulness reduces stress hormones.
This improves brain health and can lower seizure risk. Daily practice builds emotional strength. This makes stress-related seizures less likely.
Deep breathing calms your nervous system. Techniques like diaphragmatic breathing ease anxiety.
Calmness sends oxygen to the brain. This stabilizes brain activity. It avoids overstimulation.
Progressive muscle relaxation helps release body tension. You tense and then relax muscles. This reduces anxiety symptoms. It also improves sleep.
Better sleep is important for those prone to seizures.
2: Lifestyle Changes for Stress Management and Reduction of Seizures
- Sleeping on a regular schedule helps prevent seizures. Aim for seven to nine hours each night. Establish a calming bedtime routine.
- Regular exercise can also reduce seizure risk. Gentle activities like walking or swimming are good choices. Intense workouts might cause seizures.
- Eating nutritious foods benefits brain health. Foods rich in omega-3s can help balance brain chemicals. Limit coffee and sugar intake to manage stress.
3. Psychological Help for Stress-Induced Seizures
Psychological support helps people with stress seizure disorders.
- Cognitive Behavioral Therapy (CBT) is a proven therapy. It teaches coping skills to reduce negative thinking and distress. This can lower seizure risk.
- Support groups offer emotional help and advice. Connecting with others facing similar issues can build strength.
- Medical treatment is often needed for stress-induced seizures. Doctors may prescribe anti-epileptic drugs. These drugs help stabilize brain activity.
- Treating anxiety and depression is also key. These conditions can increase seizure risk. Treatments include therapy, lifestyle changes, and medication.
When to Seek Help?
Stress-related seizures must receive medical attention immediately in some cases.
You should go for medical evaluation if you have:
1: Increased frequency or severity of seizure attacks
If your seizures continue to increase in frequency irrespective of stress-reducing measures, it would be time to consult a neurologist to rule out other possible conditions.
2: Prolonged confusion or unconsciousness after a seizure
That postictal confusion is hanging around longer than simply mildly annoying and is, thus, an attractive point for consideration.
3: Severe stress that significantly impairs healthy functioning
If stress is disrupting work, relationships, or emotional well-being, one should seek assistance from a health professional to obtain relevant advice.
4: There are signs that psychogenic non-epileptic seizures (PNES) might exist
A mental health expert can look into emotional pain and past events that might cause seizure-like episodes. Getting medical help quickly can help manage the seizures better and improve life quality.
Does Stress Cause Seizures In Adults – Conclusion
The evidence strongly suggests a profound link between stress and seizure activity.
While stress may not be the sole cause, it is undeniably a powerful trigger, leading many to ask, “can tension cause seizures?”
The answer is a resounding yes, particularly in susceptible individuals.
The intricate ways stress alters brain chemistry, neurotransmitter balance, and neuronal excitability contribute significantly to seizures caused by stress and anxiety, both in epileptic and psychogenic non-epileptic cases.
Given this clear connection, prioritizing stress management isn’t just about general well-being; it’s a critical component of neurological health.
If you or someone you know experiences stress-related seizures, consult a healthcare professional like Dr. Vivek Paratp Singh (neuropsychiatrist in Patna Bihar) to develop a comprehensive stress management plan tailored to your needs.
FAQs:
1: Are Stress Seizures Dangerous?
While stress seizures themselves generally don’t directly endanger lives, they can be risky if not handled carefully.
For instance, experiencing a seizure while driving or swimming could lead to accidents or injuries.
So, managing stress levels effectively and seeking medical assistance when necessary is crucial.
Can stress seizures kill you? While stress seizures may not directly cause death, they can create hazardous situations.
For example, having a seizure while engaged in activities requiring full attention, like driving, could lead to severe accidents.
Hence, addressing stress effectively and promptly seeking medical help if you suspect stress seizures are vital for maintaining safety and well-being.
2: Can Stress Cause Seizures Without Epilepsy?
Yes, stress can trigger seizures without epilepsy, a condition known as psychogenic non-epileptic seizures (PNES).
These seizures are primarily caused by high stress, difficult situations, or severe anxiety, not abnormal brain electrical activity.
While they may resemble epileptic seizures, their root cause is emotional or psychological.
Recognizing stress as a significant trigger is crucial.
3: Can Stress Cause Epilepsy In Adults?
Stress alone does not directly cause epilepsy in adults, as epilepsy typically results from genetic, structural, or metabolic factors.
However, chronic or severe stress can trigger seizures in individuals with pre-existing epilepsy or lower the seizure threshold in susceptible people.
Conditions like psychogenic non-epileptic seizures (PNES) may also be linked to stress but are distinct from epilepsy.
4: Can Anxiety Cause Seizures Without Epilepsy?
Anxiety can cause psychogenic non-epileptic seizures (PNES). These seizures are not caused by unusual brain activity but by mental issues like stress or trauma.
PNES are different from epileptic seizures, which come from epilepsy, and doctors figure out PNES by looking at medical history and EEG tests.
Anxiety by itself does not cause epileptic seizures, but it can make symptoms worse for people who already have other conditions.
5: What Are The Symptoms Of A Stress Seizure?
What are stress induced seizures called? Stress-related seizures, often called psychogenic non-epileptic seizures (PNES), can show signs like shaking, convulsions, or being unresponsive.
They look like epileptic seizures but do not involve unusual brain activity.
Other signs can include staring, stiff muscles, or suddenly collapsing, usually caused by strong anxiety or emotional stress.
Unlike epileptic seizures, the signs of PNES can be very different and may change from one episode to another.
6: Is It Okay To Sleep After A Seizure?
Yes, it is usually safe and normal for someone to sleep after a seizure because they often feel tired or confused and need rest.
Make sure the person is in a safe position to avoid choking.
If the seizure lasted a long time, if there were many seizures, or if there are other worries like injuries or trouble breathing, get medical help before letting them sleep.

No Comments