04 Sep Hysteria Disease: What Are The Causes, Treatment And How To Cope?
Hysteria as a condition has been debated and often poorly understood throughout its medical history.
If so, you’re not alone – in fact, you’re in a company of about 6% of women who have been misdiagnosed with a common women’s health problems which has had it’s roots in superstition for years.
For literally centuries, this has been dismissed as a “female problem” that all women have to endure.
The phenomena now recognised as hysteric are, of course, described and discussed as embedded aspects of particular psychiatric and somatic entities, including conversion disorder, dissociative disorder, and psychosomatic disorder, with the term ‘hysteria’ hardly ever used in contemporary psychiatry.
This blog explores hysteria syndrome—its history, causes, symptoms, treatment options, and coping strategies—to clarify how this outdated concept relates to modern mental health conditions.
Note: Consult a psychiatrist in Patna if you or a loved one is experiencing symptoms associated with hysteria, such as excessive emotional or physical reactions.
What Is Hysteria?
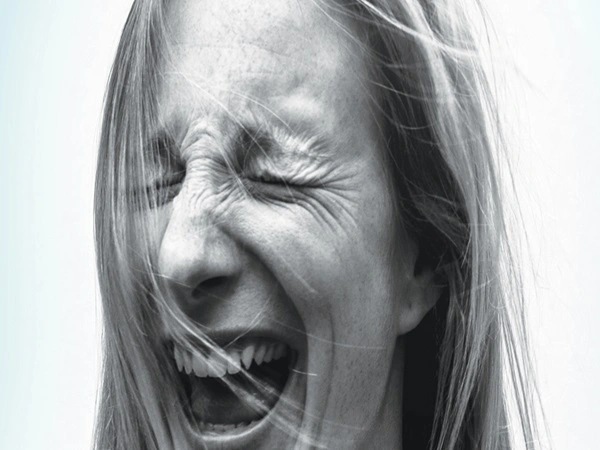
Hysteria is an archaic term once used to describe a mental health condition characterized by excessive emotional or physical reactions without a clear rational cause.
Individuals might experience sudden anxiety, fainting, tremors, temporary paralysis, or emotional outbursts.
In modern psychiatry, these hysteria syndrome symptoms are classified under conditions like:
- Conversion Disorder: Psychological stress manifests as physical symptoms, such as blindness or seizures, without a medical basis.
- Dissociative Disorder: Symptoms include amnesia or detachment from reality.
- Somatic Symptom Disorder: Chronic physical complaints lack a medical explanation.
Essentially, hysteria represents the mind’s way of expressing profound internal distress through physical symptoms.
Examples Of Hysteria
Hysteria, or more accurately, mass psychogenic illness (MPI), is the rapid spread of symptoms among a large group of people with no organic or medical basis for the symptoms.
These events are often triggered by a stressful or anxious situation and are spread through social contagion.
Here are some classic and notable examples of mass hysteria:
1. The Tanganyika Laughter Epidemic (1962)
This event began at a girls’ boarding school in Tanzania where three students started laughing uncontrollably.
The laughter spread rapidly, affecting nearly 100 students and leading to the school’s closure.
As the students went home, the “epidemic” spread, impacting hundreds in nearby villages.
Medical investigations found no organic cause, confirming it as a classic case of mass psychogenic illness.
2. The Salem Witch Trials (1692-1693)
This is a well-known example of mass hysteria fueled by fear and religious belief.
It started with a group of young women in Salem, Massachusetts, who began exhibiting strange fits and behaviors.
Their symptoms were attributed to witchcraft, leading to a wave of accusations.
This panic resulted in the unjust imprisonment of over 200 people and the execution of 20 individuals based on unproven claims.
The History of Hysteria
The concept of hysteria spans thousands of years, shaped by evolving sociocultural and medical perspectives.
Its history reflects persistent misunderstandings about mental health.
1: Ancient Egypt and Greece
The term “hysteria” derives from the Greek word hystera, meaning “uterus.”
Ancient Greek physicians, including Hippocrates, believed hysteria stemmed from a “wandering womb” that moved within a woman’s body, causing emotional and physical symptoms.
Treatments focused on reproductive health, reinforcing the idea that hysteria was exclusively a female condition.
2: Middle Ages
During the medieval period, people often attributed hysteria to witchcraft, demonic possession, or spiritual punishment.
Authorities labeled women who displayed “hysterical” behaviors—such as convulsions, fainting, or erratic energy—as witches or possessed, persecuting them instead of providing medical care.
3: 17th–18th Century
Hysteria began to be viewed as a nervous disorder rather than a female-specific condition.
It was linked to “sensitive nerves,” emotional instability, and social pressures, marking a shift toward medical rather than supernatural explanations.
4: 19th Century
The 19th century saw significant research on hysteria.
Neurologist Jean-Martin Charcot used hypnotism to study hysterical patients, while Sigmund Freud developed psychoanalysis, suggesting that hysteria resulted from unresolved psychological trauma or unconscious conflicts.
5: 20th Century to Present
The term “hysteria” was phased out of medical literature, with its symptoms reclassified under dissociative and conversion disorders. Feminist scholars critiqued the label as a historical tool to dismiss or control women’s emotional struggles.
Today, these symptoms are approached scientifically and compassionately as psychosomatic or psychological conditions.
Signs and Symptoms of Hysteria
Hysteria manifests through a combination of emotional, physical, and behavioral symptoms, often triggered by psychological stress.
These hysteria symptoms are not intentionally feigned; individuals genuinely experience distress, even without a clear medical cause.
Emotional Indicators
- Overwhelming emotional responses, such as crying, laughing, or shouting, without apparent reason.
- Sudden, intense anxiety, fear, or panic, often disproportionate to triggers.
- Difficulty managing emotions, leading to apparent instability during stressful situations.
Physical Symptoms
- Temporary paralysis, numbness, or weakness in limbs without medical explanation.
- Tremors, uncontrollable shaking, or unusual body movements.
- Sudden blindness, deafness, or loss of speech, rooted in psychological rather than neurological causes.
- Episodes resembling epileptic seizures but lacking neurological evidence.
- Chest pain, tightness, shortness of breath, or fainting during episodes.
Behavioral Indicators
- Attention-seeking behavior, such as exaggerating symptoms to gain sympathy.
- Dramatic reactions to minor stressors.
- Feelings of detachment, such as observing oneself from outside the body (depersonalization).
These symptoms highlight the complex interplay between mind and body in hysteria.
Hysteria Symptoms In Female
Female hysteria, an outdated medical diagnosis, was used to describe a wide range of symptoms, including anxiety, fainting, and emotional outbursts. The term, which comes from the Greek word for “womb,” was based on the false belief that these symptoms were caused by a “wandering uterus” or sexual deprivation.
Causes of Hysteria
Hysteria has no single cause but arises from a combination of psychological, biological, and social factors.
It often reflects the body’s response to prolonged or unresolved emotional stress.
Psychological Factors
- Unresolved Trauma: Severe experiences, such as childhood trauma abuse or loss, can trigger symptoms, especially if unaddressed.
- Repressed Emotions: Unexpressed feelings of guilt, anger, or sadness may manifest as physical symptoms.
- Acute Anxiety: Sudden, intense fear or panic can contribute to hysterical episodes.
Biological Factors
- Neurotransmitter Imbalances: Changes in brain chemistry affecting mood and emotion regulation may play a role.
- Brain Dysfunction: Dysregulation in brain areas controlling emotion, movement, or stress responses can contribute.
- Genetic Predisposition: A family history of anxiety, depression, or dissociative disorders may increase susceptibility.
Social and Environmental Factors
- Family Conflict: Ongoing disputes or dysfunctional family dynamics can destabilize emotional well-being.
- Lack of Support: Isolation or absence of a supportive network impairs emotional processing.
- Cultural Expectations: Historically, societal pressures on women contributed to the perception of hysteria.
- Mass Hysteria: In rare cases, group dynamics can lead to collective symptoms triggered by shared stress or fear.
Hysteria Treatment
Modern treatment focuses on addressing underlying psychological distress and managing symptoms through a combination of therapies and lifestyle changes.
Psychotherapy
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and replace harmful thought patterns with effective coping strategies.
- Trauma-Focused Therapy: Targets unresolved trauma contributing to symptoms.
- Hypnotherapy: Occasionally used to explore unconscious conflicts, inspired by historical practices.
Medication
- Antidepressants: Prescribed for co-occurring depression or mood-related symptoms.
- Anti-Anxiety Medications: Help manage acute anxiety or panic attacks.
- Mood Stabilizers: Used for symptoms linked to mood disorders.
Lifestyle Modifications
- Exercise: Regular physical activity reduces stress and supports mental health.
- Nutrition: A balanced diet promotes overall well-being and emotional stability.
- Stress Management: Techniques like meditation, deep breathing, or yoga help regulate emotions.
Support Systems
- Family Therapy: Improves communication and resolves family conflicts.
- Peer Support Groups: Provide a space to share experiences, reduce stigma, and learn coping strategies.
Inpatient Care
In severe cases where individuals pose a risk to themselves or others, brief hospitalization may be necessary for safety and intensive treatment.
How to Cope Hysteria Syndrome?
1: Self-Help Strategies
- Panic attacks: For calming the nervous system down and preventing panic, deep slow breathing can be a savior.
- Grounding Techniques: Interacting with an object or pet, or touching a person focuses attention and diminishes dissociation.
- Worry Log: Writing down concerns can sometimes help put them into perspective and reduce stress.
- Stress Relief: Practicing calming activities such as yoga, meditation or mindfulness can help control emotions and reduce the risk of episodes.
2: Assistance from Family and Friends
- Be Calm: Let it not infect the sufferer’s circle be allowed to get panicky; panic breeds hysteria, which is aggravated by anything else that excites.
- Comfort Them: In order to help them calm down a little, a person may finds solace in being accompanied and in a calm environment.
- Encourage Seeking Help: Instead of just ignoring the red flags and athidran, the immediate social network needs to prompt and accompany them in getting a health check done.
3: Seek Help From Psychiatrist
- Assistance via Counselling: An individual can recognize their challenges and master new helpful skills through structured counselling.
- Assistance from a Psychiatrist: Keeping a schedule of medical reviews is very important for tracking and timely changes of procedures for therapy and medication.
If someone you love is experiencing symptoms of hysteria, consider consulting with a top psychiatrist in Patna, such as Dr. Vivek Pratap Singh.
Renowned institutions like AIIMS and PMCH in Patna recognize Dr. Singh as a highly regarded neuropsychiatrist with extensive experience in neuropsychiatry, child and adolescent psychiatry, and addiction psychiatry, and he is celebrated for his compassionate and comprehensive approach to mental health care.
His clinic, Pratap Neuro and Child Psychiatry Clinic, focuses on providing specialized care for a wide range of mental health issues.
Conclusion
Although “hysteria” is no longer a formal medical diagnosis, its historical significance underscores the evolution of mental health understanding.
Once mischaracterized as a women’s disorder, it is now recognized as psychological distress manifesting through physical symptoms.
With therapy, medication, and emotional support, individuals experiencing these symptoms can lead fulfilling lives.
Awareness and compassion are key—rather than labeling or stigmatizing, we must acknowledge the complex interplay between mind and body in conditions once called hysteria.
FAQs
1. What Are The 4 Stages Of Hysteria?
Historically, scholars believed that hysteria progresses through four stages: the epileptoid stage (convulsions or seizures), the clownism stage (exaggerated or absurd movements), the attitudes passionnelles stage (emotional outbursts like sobbing or laughter), and the delirium stage (hallucinations, confusion, or detachment).
This model is no longer used in modern psychiatry but reflects historical perspectives.
2. Is Hysteria A Mental Illness?
Hysteria was historically considered a mental health condition, but the term is obsolete today.
Its symptoms are now classified under recognized disorders like conversion disorder, dissociative disorder, or somatic symptom disorder, where psychological stress manifests as physical or behavioral symptoms.
3. When Does Hysteria Start?
Symptoms typically emerge during adolescence or early adulthood, periods marked by significant emotional and social development.
However, they can occur at any age, often triggered by trauma or stress.
4. Is Hysteria Serious?
In mild forms, hysteria may disrupt daily life, affecting relationships, education, or work.
Persistent symptoms can indicate underlying trauma or anxiety, which, if untreated, may worsen.
Early intervention is crucial to prevent long-term impact.
5. How To Control Hysteria?
Managing hysteria involves self-care and professional support.
Breathing exercises and relaxation techniques reduce acute symptoms, while psychotherapy addresses root causes.
Medications like antidepressants or anti-anxiety drugs may be prescribed.
A healthy lifestyle, including exercise and good sleep, supports symptom management.
6. What Are Types Of Hysteria?
Historically, researchers divided hysteria into subtypes like conversion hysteria (physical symptoms like paralysis or sensory loss without medical cause) and anxiety hysteria (emotional symptoms like phobias or panic).
Mass hysteria describes group symptoms triggered by shared stress or social influence. These are now understood as distinct disorders.
7. What Is Female Hysteria Called Now?
The term “female hysteria” is outdated.
Modern psychiatry now classifies symptoms that were once labeled as such into somatic symptom disorder, conversion disorder, or anxiety disorders, which are not gender-specific and are better understood.
8. How Long Does Hysteria Last?
Episodes vary, lasting from minutes to hours. Without treatment, symptoms may recur over months, impacting quality of life.
Timely therapy and medical support can significantly reduce frequency and severity.
9. How To Calm Down Someone With Hysteria?
To support someone during a hysterical episode, stay calm and speak gently to reduce panic.
Encourage slow, deep breathing to ease anxiety and create a safe, low-stress environment.
Urge them to seek professional help if symptoms persist.

No Comments